You could have a secret twin (but not the way you think) - Kayla Mandel Sheets
While searching for a kidney donor,
a Boston woman named Karen Keegan
stumbled upon a mystery.
When her three adult sons
underwent genetic testing
to determine whether they were a match
for kidney donation,
the test showed that two of them
weren’t actually her sons.
Keegan knew she was her sons’ mother—
she had conceived and given birth to them.
Figuring there must have been an error,
her doctors pursued further testing,
only to uncover something
even more confusing:
she was her children’s biological aunt.
It turned out that Keegan had a second
genome in some tissues and organs.
In other words, some of her cells had
a completely different set of genes
from the others.
This second set of genes belonged
to her twin sister—
who had never been born.
This condition,
where an individual has two genomes
present in the tissues of their body,
is called chimerism.
The name comes from Greek mythology,
where chimera is an amalgam
of three different animals.
Individuals with chimerism might have
two-toned skin or hair,
or two different colored eyes,
but most are believed to have no visible
signs of the condition.
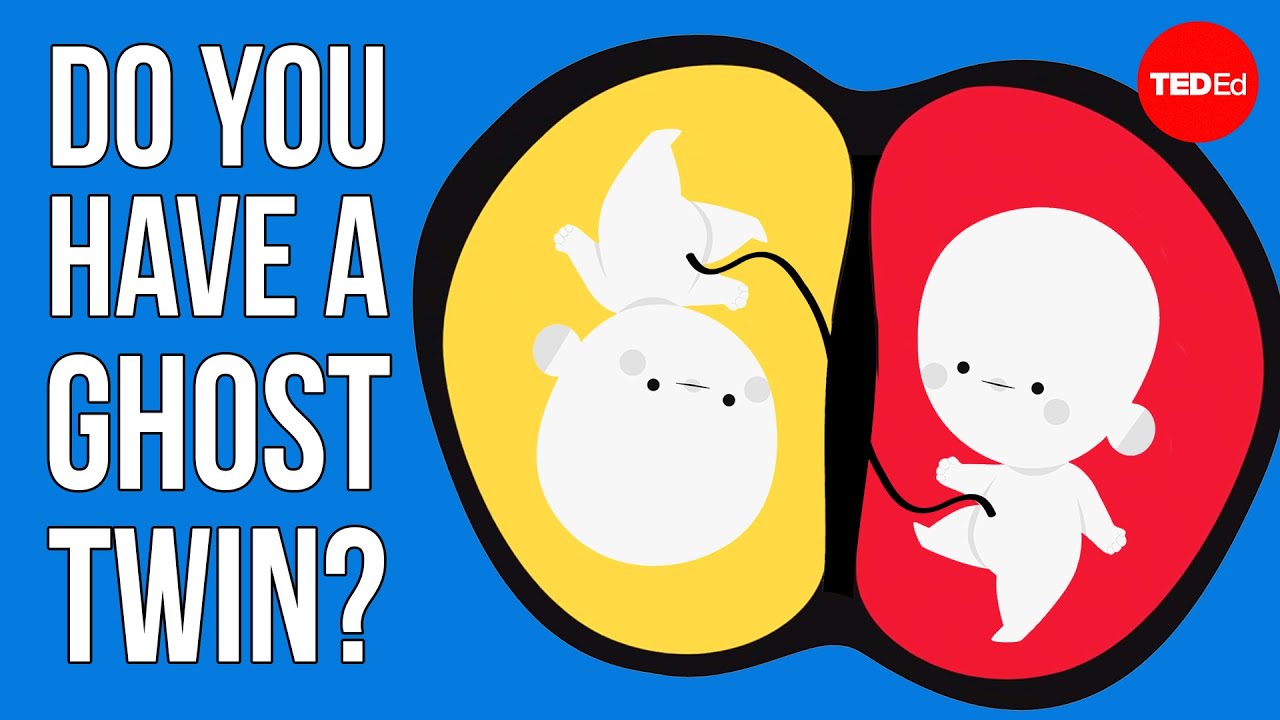
Chimerism can come from a twin in utero,
from a tissue or organ transplant,
or happen between a fetus
and a pregnant woman.
So how exactly does it happen?
In one of the most common forms,
a mother and fetus swap cells
in the flow of nutrients
across the placenta.
The mother can inherit fetal stem cells,
undifferentiated cells that are able
to develop into any specialized cell.
The fetal cells initially go undetected
because the mother’s immune system
is suppressed during pregnancy.
But in some cases, cells
with the fetus’s DNA persist
in the mother’s body
for years or even decades
without being destroyed
by her immune system.
In one case, a mother's liver was failing,
but suddenly started to regenerate itself.
Her doctors biopsied her liver,
and found DNA in the regenerated tissue
from a pregnancy almost 20 years earlier.
The fetal stem cells had lodged in her
liver and specialized as liver cells.
Karen Keegan, meanwhile, acquired
her second genome before she was born.
Very early in her own mother’s pregnancy
with her,
Keegan had a fraternal twin.
Keegan’s embryo absorbed some
fetal stem cells from her twin’s embryo,
which did not develop to term.
By the time Keegan’s fetus
developed an immune system,
it had many cells with each genome,
and the immune system recognized
both genomes as her body’s own—
so it didn’t attack or destroy the cells
with the second genome.
We don’t know how much of her body was
composed of cells with this second genome—
that can vary from one organ to another,
and even between tissues within an organ:
some might have no cells at all
with the second genome,
while others might have many.
At least some of the egg-producing tissue
in her ovaries
must have carried the second genome.
Each time she conceived there would be
no way to predict
which genome would be involved—
which is how two of her children
ended up with the genes
of a woman who had never been born.
This can also happen to fathers.
In 2014, when ancestry testing
determined that a father
was actually his baby’s biological uncle,
researchers discovered that 10%
of the father’s sperm
carried a second genome
from an embryonic twin.
Cases like this challenge
our perception of genetics.
Though there are very few documented cases
of chimerism from an embryonic twin,
we’re all amalgams to some extent,
carrying around the different genetic
codes of our gut bacteria
and even our mitochondria.
And given that 1 in 8 individual births
started out as twin pregnancies,
there could be many more people
with two genomes—
and many more lessons to learn
about the genes that make us who we are.